This post is part of the MDS 2023 Countdown series. Disclaimer. Current as of October 1, 2023
What You Can Expect to See
The reconciled medication list will have a new documentation requirement that will go into effect with the October 1, 2023 changes to the MDS 3.0. This new requirement will have an impact on a facility’s Skilled Nursing Facility (SNF) Quality Reporting Program (QRP) and Quality Measure (QM) item.
What Is Changing
This measure will assess the transfer of the reconciled medication list from the SNF to the subsequent provider, with the goal to both ensure continuity of care and minimize safety risks to the patient/resident.
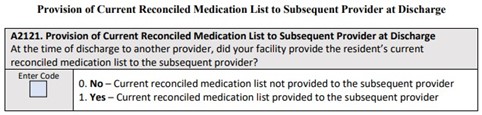
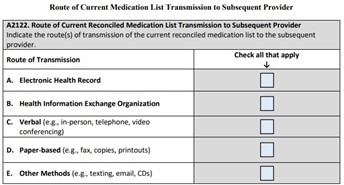
Two data elements will be used in the calculation. The single standardized patient data element (SPADE) will ask the question, “At the time of discharge, did the facility provide the patient’s/resident’s current reconciled medication list to the subsequent provider?” The second data element will ask the route of transmission the facility used to transfer the reconciled medication list.
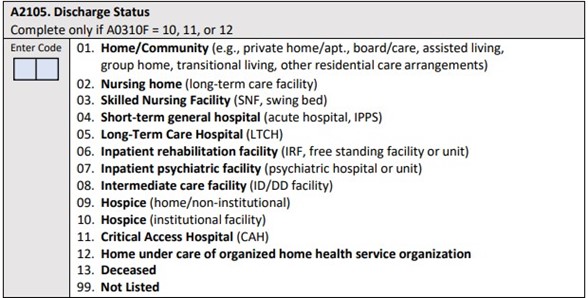
The denominator of this measure will be the number of covered SNF Medicare A residents that have a stay that ends in a discharge. This item will be coded in the updated MDS 3.0 in section A.
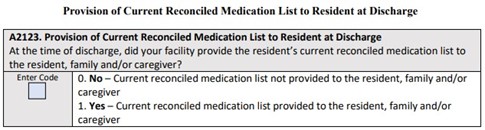
The numerator will be the number of stays that the MDS 3.0 coded item A2121 and item A2123.
This measure’s time window will be calculated quarterly and will include all SNF stays during the quarter. If a resident has multiple stays during a single quarter, each stay will be included in the measure.
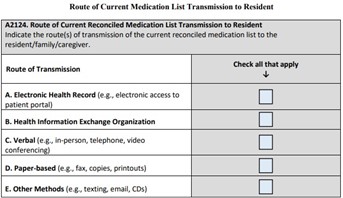
Item(s) A2122 and A2124 will code the route(s) that the current reconciled medication list was transmitted to the subsequent provider. This item is specific to patients/residents discharged to a short-term general hospital, another SNF, hospice, inpatient psychiatric facility, etc.
Recommendations from MDS Consultants
- Meet the minimum 80% completion threshold of assessments required for reporting quality measure
- Standardize patient assessment data using the MDS
- Ensure accurate and supportive documentation is present in the medical record to accurately code items A2105 and A2121-A2124 on the MDS
Starting October 1, 2023, through December 31, 2023, the SNF QRP will begin assessing and reporting on both Transfer of Health (TOH) Information to the Patient Post-Acute Care (PAC) and the TOH Information to the Provider PAC. The submission deadline for these items will be May 15, 2024.
